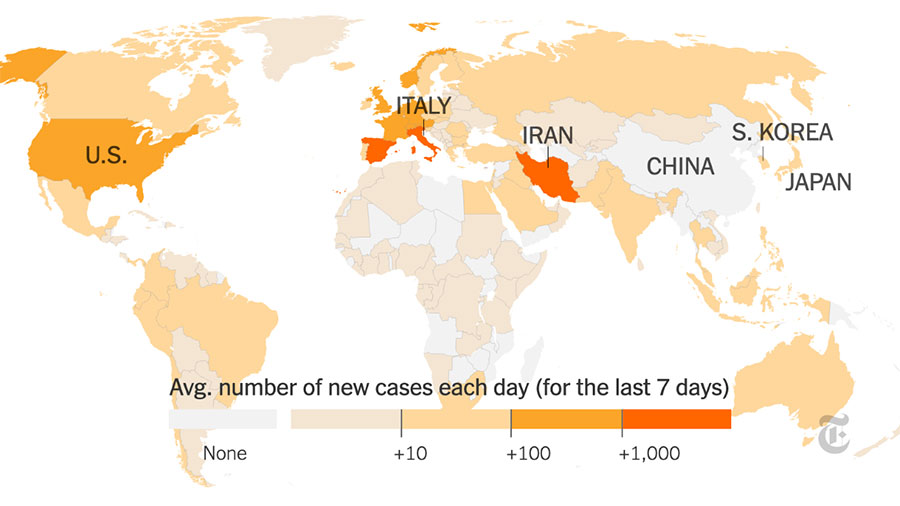
COVID-19, the current pandemic is currently spreading across the nation at a rapid rate and is causing a change in society for which many are unprepared, including social distancing, alternative academic methods and uncharted unemployment rates.
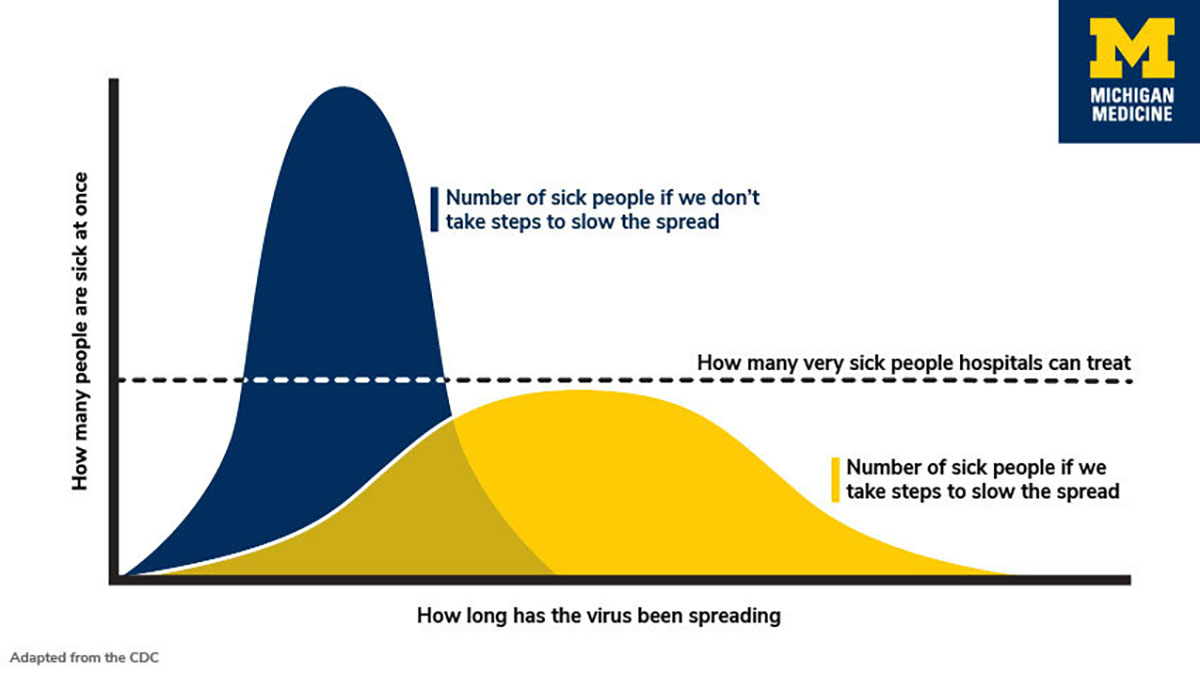
At this moment there is not much we can do, other than flattening the curve of infection to help combat the infection rates so that those with severe cases or high-risk patients have the opportunity for medical assistance.
“The No. 1 way to prevent spread is to stay home,” Kristen Wheeler, certified physician assistant in the University of Louisville-Shelbyville emergency department in Louisville, Kentucky, said. “Quarantine yourself like you’re being told. Wash your hands for 20 seconds minimum with soap and water. Use hand sanitizer with minimum of 60 percent alcohol if unable to wash hands and limit touching your face. Cover your mouth if coughing and practice good hand hygiene — stay six feet away from people.”
Self-quarantine and social distancing is necessary to “flatten the curve,” people are going to contract the virus and the main goal right now is to slow the infection rate so that more people with severe symptoms will be able to get the help that they need.
The term “flattening the curve,” refers to a curve in a chart that shows when a high rate of new coronavirus cases are expected and why slowing the spread of the infection is important because the current medical facilities are not prepared to help a mass influx of cases.
A high curve is a rapid rate of infection. A flatter slope indicates a more gradual rate of infection over a longer period. With the more gradual rate of infection more patients will be able to be treated for serious cases.
Hospitals have a limited number of rooms that are equipped to help patients with the virus, Wheeler said.
“If a patient is high risk for COVID 19 we are supposed to bring them back to a negative pressure isolation room,” she said.
If these precautions are not taken seriously the rate of infection will affect how medical facilities are able to help patients with severe symptoms. Or rather, not be able to help patients with high risk factors or symptoms.
“Those with upper respiratory infection symptoms but do not need admission, are advised to quarantine themselves at home until no longer symptomatic or until this self-quarantine issued by the government is canceled,” Wheeler said. Of course, they are advised to return to the ED if getting worse.”
Individuals who are not at high risk of the virus or have severe symptoms are suggested to treat at home and go to the emergency department if their symptoms are worsening, Wheeler said. Most of the population will not have severe symptoms and are told to stay home to help lower the chance of infecting others.
With testing kits being limited, and in most counties completely unavailable, Hospitals and emergency departments are only testing to confirm at risk and severe cases, Wheeler said.
“There is no medication to cure this — it’s a virus,” she said. “So, if you only have cold symptoms, then testing would basically be done just to say you have it but wouldn’t change anything. You don’t need to be admitted so you just need to stay home, rest, treat symptomatically, and give your body time to fight it off. If you are, if you are ill enough to be admitted, then they test.”
People who may be at higher risk with COVID-19 are older adults, people with HIV or other immunocompromising illnesses, those with asthma and pregnant women.
“Asthmatics or people with chronic pulmonary issues (lung problems) are particularly at risk as this virus seems to cause pneumonia and severe pulmonary infections,” she said. “Those with chronic lung issues will have a harder time breathing and thus surviving. COVID-19 is killing people by causing respiratory failure.”
However, younger people are not immune to COVID-19. They are still dying and are infecting others that are at higher risk. People in their 20s and 30s are being infected and are dying all over the world. The rate is much lower than the older population, but the youth are still contracting the virus and are succumbing to its symptoms.
COVID-19 is still being researched and much is still unknown about the virus. At one point it was suspected that youth were immune to the virus, and this has caused many people to not worry about the social distancing and travel precautions because they did not believe it would affect them.
The closures of airports, public places, institutions and other facilities are intended to encourage the act of self-quarantining and social distancing so that the nation can flatten the curve of infection.
During the pandemic, hospitals and other medical facilities have limited supplies that are recommended as the protective personal equipment this includes protective clothing, gowns, gloves, face shields, goggles, face masks and respirators or other equipment designed to protect the wearer from the spread of infection, Wheeler said.
“We have limited supplies of gowns and N95 masks,” she said. “We are being asked to keep the mask of suspected COVID-19 patients in a paper bag outside patients' rooms, so we do not throw them away and get a new mask each time we enter the room. We use the full PPE only if they had known exposure or traveled to endemic areas. Otherwise, a regular mask and gloves is all we wear.”
The Centers for Disease Control and Prevention does not recommend that people who are well wear a face mask to protect themselves from respiratory diseases, including coronavirus. Medical Professionals are at higher risk of direct contact with bodily fluids of suspected coronavirus patients and need the protective equipment.
A surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain germs (viruses and bacteria), keeping it from reaching one’s mouth and nose.
“Not all people with COVID-19 are going to have severe symptoms,” Wheeler said. “It’ll be like a cold and URI. There’s no way our patients (upper respiratory infection) can know if they had exposure to COVID-19 when people aren’t being tested routinely.
“So, we go in with minimal contact precautions and protective equipment on in all these ‘colds and URI’ rooms, which could still very well have the virus. We are not wearing PPE in those rooms and have numerous exposures of this type of patient throughout our shifts. We are very high risk of contracting the virus.”
Wheeler encourages everyone to stay up to date on current information about the virus, wash their hands and stay home.